Unveiling Estrogen's Crucial Role in Neurodegeneration and Neurovascular Disease Processes
Presented by Immanence Health
Written by Heathar Parisi, FNP-C
Estrogen, often associated with its role in reproductive health, holds a far-reaching influence beyond its primary functions. Emerging research sheds light on estrogen's pivotal role in neurological health, particularly its involvement in neurodegenerative and neurovascular disease processes. In this blog post, we delve into the vital relationship between estrogen and the progression of conditions such as Alzheimer's disease, Parkinson's disease, and stroke.
Estrogen and Brain Health
Estrogen receptors are abundantly present in various regions of the brain. The hypothalamus, a gland in the brain that controls body temperature, is responsible for those pesky hot flashes that more than 75% of women experience as estrogen levels fluctuate in perimenopause and into menopause. Without HRT (hormone replacement therapy), mood changes, sleep disturbances, and brain fog are also prevalent complaints during this transitional period that can persist for more than a decade. Beyond reproductive function, estrogen influences neuronal growth, synaptic plasticity, and neurotransmitter regulation. Each of these is crucial for maintaining cognitive function and preventing neurodegeneration.
The Impact of Estrogen Deficiency
Brain aging occurs alongside endocrine aging. The interactions of these processes have been implicated in cognitive decline and pathological conditions. Decreased estrogen levels in premature and natural menopause have been linked to an increased risk of neurodegenerative diseases. A growing body of research suggests that estrogen depletion exacerbates neuroinflammation, oxidative stress, and amyloid-beta deposition, contributing to the pathogenesis of Alzheimer's disease. Two of every three people diagnosed with Alzheimer’s disease are women. According to neuroscientist Lisa Mosconi, PhD, this disease actually starts in midlife, but symptoms become clinically evident in later life.
*Premature menopause may be induced surgically through bilateral oophorectomy or following chemotherapy or can be spontaneous due to premature ovarian failure (also called primary ovarian insufficiency).
Estrogen's Neuroprotective Effects
Conversely, estrogen demonstrates neuroprotective properties, potentially mitigating the progression of neurodegenerative disorders. It modulates inflammatory pathways, enhances antioxidant defenses, and promotes neuronal survival, safeguarding against neurotoxic insults. Research points to the timing hypothesis concerning the initiation of hormones as it relates to cognitive aging and the development of dementia. According to a recently published meta-analysis, it has been postulated HRT works best for the brain when used in midlife, right before or during the presence of menopausal symptoms, to minimize the architectural changes that occur as a result of hormone decline.
Estrogen and Neurovascular Function
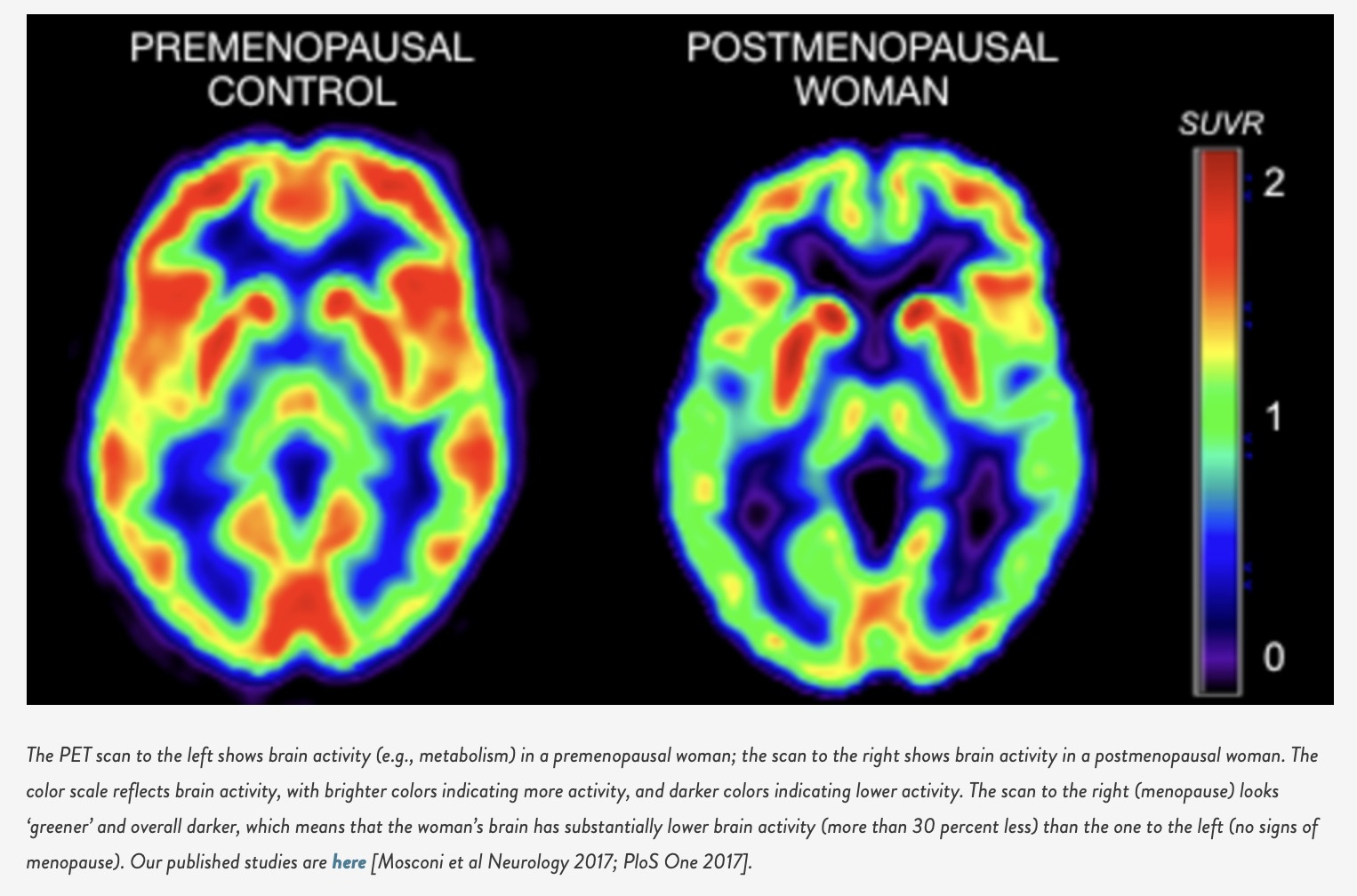
In addition to its direct effects on neurons, estrogen plays a crucial role in maintaining cerebrovascular health. Estrogen receptors are expressed in endothelial cells, where estrogen promotes vasodilation, regulates blood flow, and protects against vascular dysfunction. Disruption of estrogen signaling in the vasculature may contribute to the development of cerebrovascular diseases, including stroke and vascular dementia. The cessation of all sex hormones, particularly estradiol, precipitates a biochemical shift due to a lack of receptor activation. As a woman transitions into menopause, she may lose around 30% of her brain’s energy levels. This results in reductions of neuronal concentrations and connectivity, decreases in blood flow, and alterations of grey matter.
Estrogen Therapy and Neurological Disorders
Given estrogen's confirmed and very complex influence on brain health, hormone replacement therapy has garnered interest as a potential intervention for neuroprotection. The therapeutic use of MHT* (menopausal hormone therapy) is a viable consideration in clinical practice. Providers must consider timing, type of HRT, and individual risk factors. While some studies reveal the benefits of HRT in reducing the risk of cognitive decline and stroke, others, including two recent randomized trials (WHIMS-Y and KEEP-Cog), showed neither harm nor benefit of HRT interventions in postmenopause. These contradictions highlight the need for further research and, as always, personalized approaches with each individual. Context is everything, and specialized cardiovascular testing is integral to the structuring of the protocol when women have been away from sex hormones for ten years or more. As we are learning, neurodegenerative diseases are multifaceted and have no one-size-fits-all approach. Excess inflammation, metabolic derangement, mitochondrial dysfunction, and poor nutrient status are all hallmarks of neurodegeneration and need to be evaluated and addressed along with hormone decline. Dr. Dale Bredesen’s recently published study, "Precision medicine approach to Alzheimer’s disease: Successful pilot project." His team used in-depth diagnostics to assess each patient’s genetics and biomarkers, including hormone status, to design a precision medicine protocol. After nine months of these interventions, clinical trial results showed that 84% of participants had a moderate reversal of cognitive decline and improved cognitive function and performance.
*MHT (menopausal hormone therapy) and HRT (hormone replacement therapy) are terms used interchangeably but mean the same thing.
Conclusion
The intricate interplay between estrogen and neurological health underscores its significance in understanding and potentially intervening in neurodegenerative and neurovascular disease processes. Further research into estrogen's mechanisms of action and the development of targeted therapies is currently ongoing and may offer novel strategies for preserving brain function and combating age-related cognitive decline and cerebrovascular disorders. By unraveling the complexities of estrogen's role in the brain, we pave the way for future advancements in neurological healthcare and the pursuit of effective treatments for these debilitating conditions.
Additional Sources:
- Mosconi L, Walters M, Sterling J, et al. Lifestyle and vascular risk effects on MRI-based biomarkers of Alzheimer's disease: a cross-sectional study of middle-aged adults from the broader New York City area. British Medical Journal (open access) 2018; http://dx.doi.org/10.1136/bmjopen-2017-019362.
- Girard, R., Météreau, E., Thomas, J. et al. Hormone therapy at early post-menopause increases cognitive control-related prefrontal activity. Sci Rep 7, 44917 (2017). https://doi.org/10.1038/srep44917
- Toups, Kat et al. ‘Precision Medicine Approach to Alzheimer’s Disease: Successful Pilot Project’. 1 Jan. 2022 : 1411 – 1421. DOI: 10.3233/JAD-215707
- Conde DM, Verdade RC, Valadares ALR, Mella LFB, Pedro AO, Costa-Paiva L. Menopause and cognitive impairment: A narrative review of current knowledge. World J Psychiatry. 2021 Aug 19;11(8):412-428. doi: 10.5498/wjp.v11.i8.412. PMID: 34513605; PMCID: PMC8394691.
- Nerattini, M., Jett, S., Andy, et al. (2023). Systematic review and meta-analysis of the effects of menopause hormone therapy on risk of Alzheimer’s disease and dementia. Frontiers in Aging Neuroscience, 15. https://doi.org/10.3389/fnagi.2023.1260427
- "Evidence That Early Alzheimer’s Can Be Reversed - Bredesen Protocol Clinical Trial Results," : https://www.apollohealthco.com/alzheimers-reversal/
About Heathar Parisi, FNP-C
Advanced Nurse Practitioner, Heathar Parisi, is a women’s health and hormone expert. As a family nurse practitioner, herbalist, and functional medicine provider, she uses a holistic approach when treating women in perimenopause and menopause, always keeping connection and humor as the centerpiece of her interactions. She has specialty training in the Menopause Method for the use of BHRT through the Institute of Bioidentical Medicine (IOBIM). She is a mother of three and resides in Scottsdale, AZ with her family. Consultations are available through Immanence Health.
To learn more about working with
Heathar Parisi, FNP-C
in person or virtually (US and Worldwide), set up a free discovery call with our team.
Disclaimer: this post is for informational purposes only and is not meant to treat, diagnose, cure, or prevent any disease. Please do your own research and consult with your own personal licensed health care provider before making any treatment decisions.
Share Article

Dr. Christine Schaffner
Founder / Physician
Dr. Schaffner is a board-certified Naturopathic Doctor and recognized thought leader. After graduating from Bastyr University in Seattle, Washington, Dr. Schaffner completed her undergraduate studies in Pre-medicine and Psychology at the University of Virginia in Charlottesville.
With her diverse skill set, Dr. Schaffner seeks to improve access, outcomes, and speed of recovery for patients struggling with chronic illness, from all around the world and combines both naturopathic and conventional therapies to develop individualized treatment plans that focus on addressing the underlying cause of complex chronic illness.
Dr. Schaffner is passionate about educating patients, as well as other practitioners, bringing the most advanced medical protocols to all, as well as creating spaces for healing and rejuvenation. Her style of practice is strongly rooted in traditional naturopathic principles, including removing toxins and establishing a strong health foundation in order to achieve optimal health.
You can learn more about Dr. Schaffner at www.drchristineschaffner.com.
Additional Articles